
Drinking alcohol when on antibiotics: A Complete Guide
Let’s get right to it: can you drink alcohol while taking antibiotics? The simple, straightforward answer is no. It’s a risk that just isn’t worth taking. With certain antibiotics, the combination is genuinely dangerous. With others, it can seriously sabotage your body’s ability to heal.
The Real Risks of Mixing Alcohol and Antibiotics

When you’re sick, your body is already working overtime to fight off an infection. Think of your system as a dedicated repair crew, and the antibiotics are the specialized tools they need to do the job right. Introducing alcohol is like throwing a wrench in the works—it distracts the crew, slows down the repairs, and can even cause new problems.
Even if a specific antibiotic doesn’t trigger a severe, immediate reaction with alcohol, the mix is still a bad idea. It puts unnecessary stress on your body precisely when it needs every ounce of energy for healing. Let’s break down exactly why this combination is a problem.
Why Your Body Needs a Break from Alcohol
Skipping alcohol while on antibiotics isn’t just about dodging a scary drug interaction. It’s about giving your body the best shot at a full and fast recovery. The issues go far beyond just what happens when the two substances meet in your stomach.
The truth is, alcohol can mess with everything from how your body processes the medication to how well your own immune system can do its job. It’s well-known that alcohol weakens immune function, hobbling the very cells that are supposed to be fighting the infection. On top of that, drinking while you’re sick can make the common side effects of antibiotics—like an upset stomach, dizziness, or drowsiness—feel so much worse.
So, while the medication is trying to knock out the bad bacteria, alcohol is actively undermining your body’s natural defenses.
The Two Primary Dangers
When you look at the risks of drinking on antibiotics, they really boil down to two major problems. Both can compromise your health and drag out your illness.
- Intensified Side Effects: Many antibiotics can cause side effects like nausea, stomach pain, and dizziness all on their own. Alcohol can crank the volume way up on these, turning a minor annoyance into a miserable experience.
- Reduced Treatment Effectiveness: Alcohol can interfere with how your body, especially your liver, breaks down the medication. It also suppresses your immune system, making it that much harder for your body to win the fight against the infection, even with the help of the antibiotic.
Choosing to pause drinking isn’t just a precaution—it’s an active decision to support your body’s healing process. This short break can even shine a light on some of the amazing benefits of sobriety, even if it’s just for a week or two.
How Alcohol Sabotages Your Antibiotic Treatment
When you’re sick enough to need antibiotics, your body is already working overtime to fight off a bacterial infection. Think of the antibiotic as a crucial ally in that fight. Pouring alcohol into the mix doesn’t just fail to help; it actively undermines your recovery on several fronts.
The problems range from making you feel much worse to seriously interfering with how your body processes the medication. It puts extra strain on your immune system and your liver, right when they need to be at their best.
Turning Side Effects from Bad to Worse
Most antibiotics have a list of potential side effects—things like nausea, dizziness, or just feeling a bit drowsy. Usually, these are mild and manageable.
But alcohol often causes those exact same symptoms. When you combine them, you’re not just adding the effects together; you’re multiplying them. A little bit of drowsiness from your pill can turn into overwhelming fatigue after just one beer. Mild nausea can quickly become intense vomiting, which dehydrates you and makes it even harder for your body to heal. It’s a recipe for turning a manageable sickness into a truly miserable experience.
Weakening Your Immune System
Your antibiotics are powerful, but they’re not magic. They’re designed to assist your immune system, not do the entire job for it. Your body’s own defenses are still the main force fighting to clear out the infection.
Here’s the problem: alcohol is a well-known immune suppressant. It slows down your body’s natural ability to fight off invaders. This means your antibiotics are left trying to do a much harder job with less backup, which can drag out your illness and make you feel sick for longer than you need to.
It’s like your immune system and the antibiotics are a team working together. Alcohol is the teammate who shows up and starts distracting everyone, leaving the antibiotics to try and handle the entire workload alone.
Overloading Your Liver
This is where the most direct and potentially dangerous interaction happens. Your liver is your body’s primary processing plant. When you take an antibiotic, your liver gets to work metabolizing it—breaking it down so your body can use it and then flush it out.
Now, imagine you pour alcohol into that system. Your liver sees alcohol as a toxin and prioritizes getting rid of it immediately. This creates a metabolic traffic jam. Suddenly, your liver has to process both the drug and the drink at the same time, leading to two major issues:
- The Antibiotic Might Not Work: If the liver is busy with alcohol, it might metabolize the antibiotic incorrectly. The drug could get broken down too fast, preventing its concentration from ever getting high enough in your bloodstream to effectively kill the bacteria.
- You Could Strain Your Liver: Forcing your liver to handle both substances is incredibly stressful for the organ. This can lead to inflammation and, with certain antibiotics, increase the risk of liver damage.
This is the core reason why drinking alcohol when on antibiotics is such a bad idea. You’re potentially making your medication less effective while putting a vital organ under unnecessary stress.
On top of all this, both antibiotics and alcohol can mess with the delicate balance of your gut microbiome. For a deeper dive into this, you can learn more by understanding gut health. The bottom line is clear: skipping alcohol is a simple, powerful step you can take to help your body heal and ensure your treatment works as it should.
Antibiotics You Should Never Mix with Alcohol
When you’re sick, the last thing you want is to make things worse. But that’s exactly what can happen if you mix alcohol with certain antibiotics. Not all antibiotics react with alcohol in the same way, and understanding the difference is crucial for your safety. While it’s always a good idea to skip the drinks while you’re on medication, some combinations are downright dangerous.
Think of it like a traffic light system. Some antibiotic-alcohol pairings are a hard red light—stop immediately. Others are a yellow light, demanding serious caution. And a few are more like a green light, but with a warning sign attached.
High-Risk Zone: Do Not Mix
Let’s start with the non-negotiables. A handful of antibiotics fall into a strict “do not mix” category. Drinking alcohol while taking these can trigger a violent physical response known as a disulfiram-like reaction. This isn’t just about feeling a little off; it’s a severe, full-body reaction that can happen within minutes of your first sip.
This reaction happens because the antibiotic blocks a key enzyme your liver needs to process alcohol. As a result, a toxic compound called acetaldehyde builds up in your system, causing a cascade of miserable symptoms.
The main culprits here are:
- Metronidazole (Flagyl): Perhaps the most notorious on this list, it’s often used for dental work, stomach bugs, or vaginal infections.
- Tinidazole (Tindamax): Similar to metronidazole, this drug is used for certain parasitic and bacterial infections and carries the same severe risk.
- Cefotetan: An injectable antibiotic from the cephalosporin family that can also trigger this intense reaction.
A disulfiram-like reaction is no joke. Symptoms are immediate and include intense nausea and vomiting, a pounding headache, flushed skin, a racing heart, and shortness of breath. It’s your body’s way of sending a crystal-clear message: stop.
Moderate-Risk Zone: Proceed with Caution
Next up are the “moderate risk” antibiotics. These won’t typically cause the same violent reaction as the high-risk group, but mixing them with alcohol can still create major problems. We’re talking about everything from dangerous spikes in blood pressure to making the usual side effects feel much, much worse.
A global study highlighted that antibiotics like metronidazole, tinidazole, and sulfamethoxazole-trimethoprim have a strong negative interaction with alcohol, causing reactions like flushing, headaches, and nausea. For some, like linezolid, the danger comes from specific types of alcohol. You can discover more about these medication interactions from Parkview Health.
Keep an eye out for these medications:
- Sulfamethoxazole-trimethoprim (Bactrim, Septra): While the risk is lower than with Flagyl, some people still report similar, though milder, reactions.
- Linezolid (Zyvox): This one can interact with tyramine-rich alcoholic beverages—think red wine and tap beer—leading to a dangerous jump in blood pressure.
- Ketoconazole: This antifungal already puts your liver to work. Adding alcohol into the mix significantly increases the risk of liver damage.
This infographic shows just how alcohol can mess with your treatment, from amplifying side effects to weakening your body’s ability to fight off the infection.
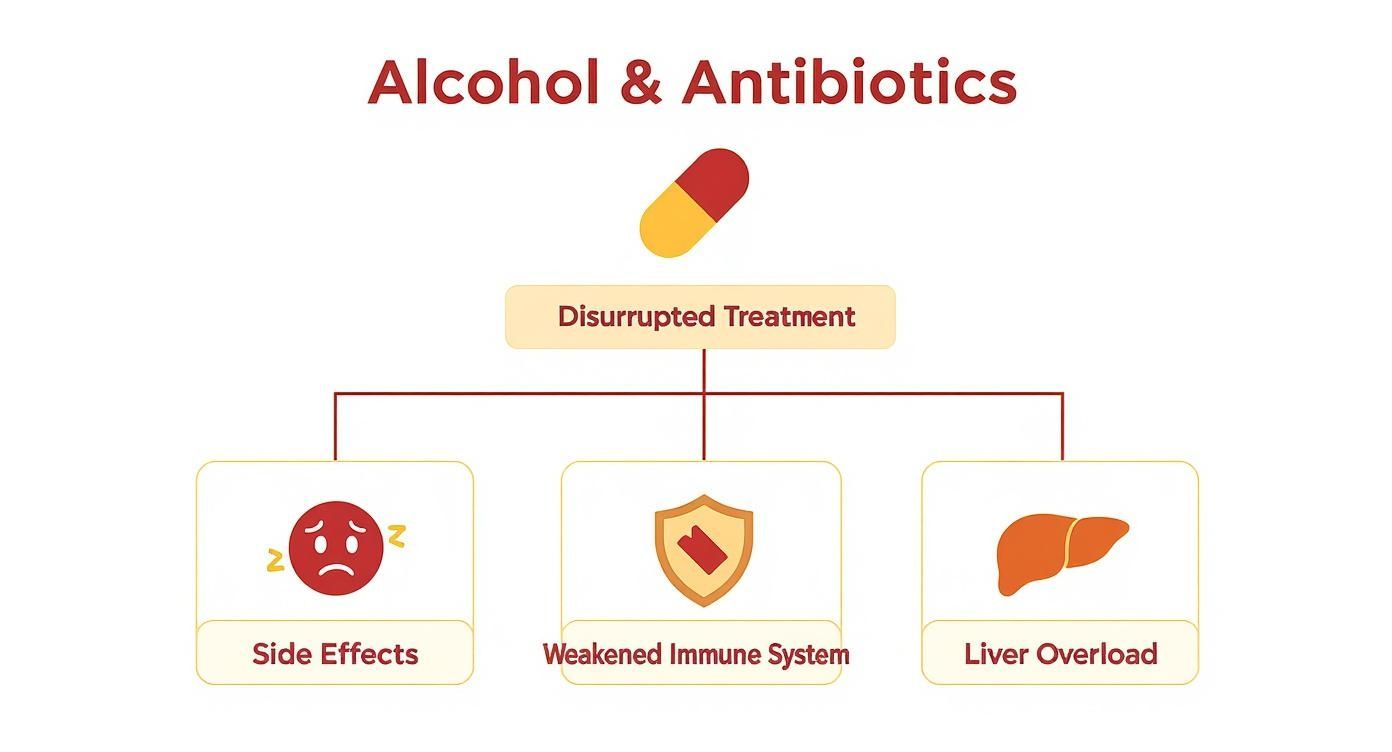
As you can see, it’s not just one issue. It’s a combination of factors that all get in the way of your body’s ability to heal.
Lower-Risk Zone: Still Best to Avoid
Finally, we have the “lower risk” category, which includes many of the most commonly prescribed antibiotics like amoxicillin and doxycycline. A severe, life-threatening reaction from having a single drink with these is highly unlikely.
But “lower risk” absolutely does not mean “no risk.” Alcohol can still make the common side effects of these drugs feel a lot worse. You might experience:
- Stomach upset and nausea
- Dizziness and drowsiness
- Diarrhea
Plus, regardless of the antibiotic, alcohol can put a damper on your immune system and slow down your recovery. Your body is already working overtime to get better. Why add another stressor to the list? The smartest and safest choice is always to just wait until you’ve finished your prescription and are feeling back to 100%.
Antibiotic and Alcohol Interaction Risk Levels
To make it easier, here’s a quick-glance table summarizing which antibiotics to be most careful with.
| Risk Level | Antibiotic Examples (Brand Names) | Potential Reactions with Alcohol |
|---|---|---|
| Severe | Metronidazole (Flagyl), Tinidazole (Tindamax), Cefotetan | Disulfiram-like reaction: Severe nausea, vomiting, flushing, headache, racing heart, shortness of breath. |
| Moderate | Sulfamethoxazole-trimethoprim (Bactrim), Linezolid (Zyvox) | Milder disulfiram-like symptoms; dangerous blood pressure spikes (especially with tyramine-rich drinks like red wine). |
| Moderate (Organ Strain) | Ketoconazole (Nizoral) | Increased risk of liver inflammation and damage. |
| Low | Amoxicillin (Amoxil), Doxycycline (Vibramycin), Ciprofloxacin (Cipro) | Worsened side effects like nausea, dizziness, and stomach upset; reduced immune function. |
This chart is a helpful guide, but it’s not a substitute for medical advice. Always check with your doctor or pharmacist about your specific prescription before even considering a drink.
What to Do If You Have an Adverse Reaction

Even with the best of intentions, slip-ups can happen. Maybe you forgot you were on medication or simply didn’t know about the risks until after you’d already had a drink. If you start feeling sick after drinking alcohol on antibiotics, the first rule is: don’t panic. What’s important is knowing how to read your symptoms and what to do next.
Figuring out if you’re having an adverse reaction is the first critical step. These reactions can be anything from mildly unpleasant to genuinely dangerous, so being able to tell the difference is key to keeping yourself safe.
Recognizing Mild Symptoms
Most reactions fall into the mild category. They’re no fun, but they usually aren’t a full-blown medical emergency. Think of it as the normal side effects of alcohol or the antibiotic, but turned up to eleven.
Keep an eye out for these more common, milder signs:
- Facial Flushing: Your face, neck, or chest might get red, splotchy, and feel warm to the touch.
- Increased Dizziness or Drowsiness: You could feel way more lightheaded or sleepy than you normally would from that amount of alcohol.
- Nausea or Stomach Upset: That queasy, unsettled feeling in your stomach might show up or get worse.
If you notice any of these, the most important thing to do is stop drinking immediately. No more alcohol. Switch to water to stay hydrated, find a comfortable spot to rest, and just monitor how you feel. In most cases, these symptoms will fade as your body processes the alcohol.
It’s also worth remembering that antibiotics alone can mess with your gut. If you’re dealing with general discomfort, some natural remedies for digestive issues could help bring some balance back once the immediate reaction has passed.
Identifying Severe Reaction Red Flags
Sometimes, especially with high-risk antibiotics like metronidazole, the reaction can be much more severe. These symptoms are your body’s alarm bells, signaling a potential medical emergency that needs attention right away.
Do not wait to see if severe symptoms improve on their own. A serious disulfiram-like reaction can escalate quickly and requires professional medical care. Your safety is the top priority.
Knowing these red flags could literally save a life. If you or someone else has any of the following symptoms after drinking on antibiotics, it’s time to get help—fast.
Emergency Symptoms Requiring Immediate Medical Attention
- Severe Pounding Headache: We’re not talking about a regular headache. This is a sudden, intense, and throbbing pain.
- Chest Pain or Pounding Heartbeat: Any feeling of pressure, tightness, or pain in your chest is a major warning. So is a heart that feels like it’s racing, fluttering, or pounding out of your chest (palpitations).
- Difficulty Breathing: Feeling winded, wheezing, or like you just can’t get a full breath in.
- Severe Vomiting: Intense, non-stop vomiting that makes it impossible to even keep water down.
- Confusion or Extreme Weakness: Feeling disoriented, incredibly weak, or like you can’t stand up on your own.
If you spot any of these severe signs, call for emergency medical help immediately. Don’t try to drive yourself to the hospital. When you call, be ready to tell the paramedics exactly which antibiotic you’re on and how much alcohol you drank. Acting quickly is the most important thing you can do.
How Long to Wait After Antibiotics to Drink Alcohol
So, you’ve taken the final pill in your prescription. The obvious question pops into your head: when is it actually safe to have a drink? It’s tempting to celebrate feeling better, but your body is still on the clock, processing the medication and finishing the healing process. There’s no one-size-fits-all answer here; it really comes down to the specific antibiotic you were taking.
The crucial factor is the drug’s half-life. This is just a clinical term for the time it takes your body to break down and get rid of half of the drug. Some antibiotics are in and out of your system pretty quickly, while others can hang around for days, still working long after your last dose.
The Non-Negotiable Waiting Period for High-Risk Drugs
For antibiotics in the high-risk group—we’re looking at you, metronidazole and tinidazole—the waiting period is absolutely non-negotiable. You have to be strict about this one. These drugs can trigger a nasty disulfiram-like reaction if they’re still in your system when you drink alcohol.
Because of this risk, standard medical advice is to wait at least 72 hours (that’s three full days) after your final dose before even thinking about alcohol. This gives your body enough time to completely clear the medication, so you don’t set off the intense nausea, vomiting, and heart palpitations that come with this interaction. Think of it as a mandatory cool-down period to prevent a serious system overload.
General Guidelines for Other Antibiotics
For most other common antibiotics, the main concern is less about a severe chemical reaction and more about making side effects worse or hindering your immune system. In these cases, a general guideline is to wait at least 48 hours (two days) after your last dose.
This 48-hour buffer does two important things:
- It lets the medication fully exit your system.
- It gives your body a little extra time to recover from the infection itself.
Remember, the antibiotics dealt with the bacteria, but your immune system is still on clean-up duty, repairing the damage. Giving it a couple of alcohol-free days helps you get fully back on your feet and lowers the risk of a relapse. The journey to wellness doesn’t end with the last pill; it extends through the initial stages of recovery. For a deeper look into what this process entails, exploring an alcohol recovery timeline can offer valuable insights into how the body heals.
Your safest bet is always personalized medical advice. Before you drink, a quick call to your doctor or pharmacist can provide a definitive answer based on your specific prescription, dosage, and overall health profile.
Interestingly, a systematic review of alcohol warnings found that many common antibiotics, like penicillins and azithromycin, can often be taken with moderate alcohol consumption without causing severe reactions or losing their punch. However, the same review pointed out that other drugs, like erythromycin and doxycycline, could be less effective when mixed with alcohol, especially for chronic drinkers. Read the full research about these antibiotic findings to understand why expert advice is so important.
Listen to Your Body Above All Else
Ultimately, the best advice is to simply listen to your body. Even after the recommended waiting period is over, you might still feel worn out from being sick. Your body has just been through a fight, and jumping back into old routines too fast can set you back.
If you’ve waited the right amount of time but still don’t feel 100%, maybe hold off on that drink for another day or two. Making your full recovery the priority is always the smartest move. The goal isn’t just to be infection-free; it’s to be genuinely well.
Common Questions About Alcohol and Antibiotics
Taking a course of antibiotics can raise a lot of questions, especially when it comes to daily life—like whether it’s okay to have a drink. The advice out there often feels confusing or even contradictory, leaving people wondering what’s actually safe. Let’s clear up the confusion and give you some straightforward answers to the most common questions about mixing alcohol and antibiotics.
My goal here is to cut through the noise and give you practical, no-nonsense information so you can make smart, healthy choices while you get better.
What If I Accidentally Had One Drink on Antibiotics?
First off, don’t panic. It happens more often than you’d think, and a single, accidental drink isn’t usually a medical emergency. What happens next really depends on which antibiotic you’re taking.
If you’re on a common antibiotic with a lower interaction risk, like amoxicillin, one drink is highly unlikely to cause a severe reaction. You might, however, feel the usual side effects—like drowsiness or an upset stomach—a bit more intensely. The best thing to do is to stop drinking right away, switch to water, and just keep taking your medication exactly as your doctor prescribed.
But if you’re on a high-risk antibiotic like metronidazole, the situation is more serious. You’ll need to watch yourself closely for symptoms like facial flushing, a pounding headache, nausea, or a racing heart. If you notice any of these signs, and they feel severe, it’s a good idea to get medical advice. No matter what, don’t have another drop of alcohol.
Can Drinking Alcohol Make My Antibiotics Less Effective?
Yes, it absolutely can, and this is a risk people often underestimate. While alcohol might not completely cancel out your medication, it can definitely get in the way of your treatment and slow down your recovery.
It all starts with your liver. Your liver is responsible for processing both the alcohol you drink and the antibiotic in your system. When you drink, your body treats alcohol as a toxin and prioritizes breaking it down first. This can mess with how the antibiotic is metabolized, sometimes flushing it out of your system too quickly before it can build up to the levels needed to kill off the infection.
Even more importantly, alcohol is a known immune suppressant. Your antibiotics are there to help your immune system fight the infection, not to do all the work on their own. Drinking weakens your body’s natural defenses, which means you’re forcing the medication to do all the heavy lifting. This can make you feel sick for longer and drag out your recovery.
Does This Warning Apply to All Alcoholic Drinks?
You bet. When we say avoid alcohol, we mean all of it. The warning applies to any beverage containing ethanol, which includes beer, wine, hard seltzers, and any kind of liquor. The problematic interaction is with the alcohol molecule itself, not the other ingredients.
It’s also smart to be aware of hidden sources of alcohol. Some common household products contain enough alcohol to trigger a reaction, especially with those high-risk antibiotics. Always check the labels on things like:
- Mouthwash: Many popular brands are surprisingly high in alcohol content.
- Certain cold and cough syrups: Take a look at the “inactive ingredients” list.
- Some food preparations: Dishes made with cooking wine or liqueurs can retain some alcohol.
With certain antibiotics like linezolid, the risk gets even more specific. It can react badly with tyramine-rich drinks like red wine and tap beers, leading to a dangerous spike in blood pressure. The simplest, safest rule is just to steer clear of all alcohol until your treatment is finished and you’re feeling better.
Why Didn’t My Doctor Warn Me About Drinking?
That’s a really common and fair question. Think about how fast a typical doctor’s appointment goes. Your doctor is focused on the most critical information—how often to take the pill, why it’s vital to finish the entire prescription, and what major side effects to look for. They might simply overlook mentioning alcohol, especially if the antibiotic they’ve prescribed has a lower risk of a severe interaction.
Sometimes, doctors assume the pharmacist will cover those details when you pick up your prescription. And legally, the patient information leaflet that comes with your medication will always list potential drug interactions, including alcohol.
Still, just because you didn’t get a verbal warning doesn’t mean it’s safe to drink. The best thing you can do is be your own health advocate. Anytime you get a new prescription, make it a habit to ask your doctor or pharmacist directly, “Is there anything I should avoid eating or drinking while I’m taking this?” That one simple question ensures you have the full picture.
For those who find that drinking is a recurring issue when they’re sick, understanding the first steps toward recovery can be empowering. Our guide on how to quit drinking offers practical advice for anyone thinking about making a change.
If you’re looking for support to manage your relationship with alcohol, whether during a short-term illness or for the long haul, Soberly is here to help. Our app provides tools to track your progress, build healthy habits, and connect with a community that understands. Take control of your health journey by downloading Soberly today at https://getsoberly.com.